The appointment starts with great promise.
The neurologist, young and eccentric, says he knows exactly how to help my daughter. Follow his recommendations, he says, and she’ll be talking, using the toilet and behaving like a typical five-year-old in no time.
I am giddy with relief.
It’s a feeling all special needs parents know well. In a world where no one “gets” our kids — and some just get them flat-out wrong — when you encounter someone who not only gets them but knows how to help them, it’s like Christmas, your birthday and the season premiere of The Walking Dead all in one.
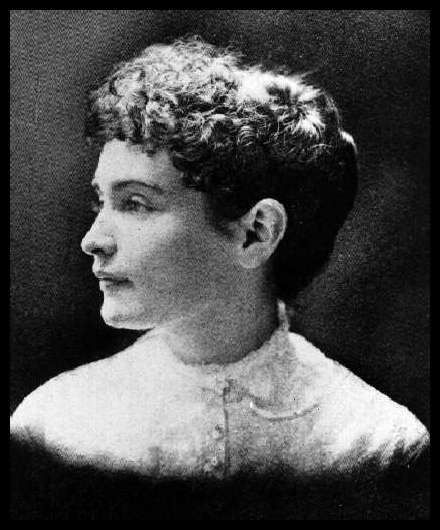
I call it the Annie Sullivan Effect, for the woman who taught a blind and deaf Helen Keller how to communicate. Like Sullivan, these women and men come into your child’s life and flip a switch you didn’t even know where to look for.
We have been lucky enough to know several Annie Sullivans. They hold a special place in our hearts and prime real estate in our prayers.
But as much as I adore these people, there is a massive drawback to meeting a real life Annie Sullivan. It makes the disappointment that much greater when someone who appears to have Sullivan potential turns out to be a JAGBA, (Just Another Giver of Bad Advice).
If there is one thing special needs parents have in abundance it’s JAGBAs. They leap out at us whenever we venture forth in public with our children or post about them on social media.
“Do you speak with him?” one woman asked when I explained that my then-3-year-old son couldn’t talk. “I mean, maybe if you modeled speech it would help.”
I was beyond tempted to reply, “No, we communicate entirely in mime. Look! He’s doing the ‘I’m-trapped-in-a-giant-invisible-box’ routine! Haha. Good one, buddy!”
While JAGBAs exist for all moms and dads, they can be particularly vexing for special needs parents because, unless the person speaking has a degree in neurologically atypical development, he or she has about as much chance of giving appropriate advice as I do of being crowned Miss Argentina. (It could happen but the circumstances would be very suspicious.)
Even once you do explain your child’s condition, some JAGBAs refuse to accept that this negates their words of wisdom. That some kids are wired differently challenges, well, apparently everything they believe about the universe.
Having seen up close and personal how differently some children develop, I can very comfortably say it is more bizarre to believe the “one-size-fits-all” line of thinking than it is to reject it.
Take my son and speech. Everything that helped typical kids learn how to speak, such as modeling speech, didn’t work for him. And trust me, we modeled out the wazoo. At his pediatrician’s request I narrated everything we did, much to the concern of people who found themselves near us in public. “Here we go up the stairs,” I’d say, as people inched away from the crazy lady. “Up, up, up the stairs.”
Even things that helped the majority of atypical kids learn how to speak, such as speech therapy and sign language, didn’t work. (And no, despite what some JAGBAs argue, learning sign language does not discourage kids from speaking. It’s not like they have the keys to the kingdom being able to sign “milk” and “potty.”)
So what did the trick? A new neurologist and an occupational therapist who determined the problem was with my son’s vestibular system. (Essentially, his sense of balance.) Instead of trying to get him speak, this therapist focused on movement. She pushed him on platform swings and swung him in circles. Within a week, he said his first words. Probably to get her to stop.
When you witness something like this, you don’t just drink the neurologically atypical Kool-Aid, you chug it.
That’s why I am ready to follow every recommendation this young neurologist gives. He has already built a reputation within the local special needs community for “thinking outside the box” and getting results.
His first suggestion is to take a stool sample so he can prescribe a course of probiotics and supplements for my daughter. Sounds good.
He then sends us across the hall so his nutritionist can devise a special diet for her. I am THRILLED. Eating has been a major issue for my daughter ever since she started chemotherapy and the constant nausea and vomiting turned her off food.
Toward the end of her cancer treatment she was fed entirely through a tube. When she began her recovery, her doctors recommended a liquid meal replacement drink to help her gain weight and grow as we gradually reintroduced solid foods. It has helped us tremendously but we would love nothing more than for her to enjoy eating again.
Unfortunately, the nutritionist is no Annie Sullivan.
The trouble starts when this woman — let’s call her Twiggy — enters the room, turns sideways and disappears. Okay, I’m exaggerating but she was worryingly skinny. I know it’s not nice to be prejudiced against anyone for their weight but I have a really hard time trusting anyone who doesn’t seem to enjoy food. Especially a nutritionist. I mean, what was she going to teach my daughter to eat? Altoids and laxatives?
She asks for a list of foods that my daughter consumes on a regular basis. It’s a short list and when I mention the name of the supplement beverage, her head snaps up and her eyes grow wide over protruding cheek bones.
“That stuff is poison,” she says. “It’s full of sugar and sugar feeds cancer.”
“Her oncologist recommended it,” I reply. “Her tumors have been steadily shrinking the entire time she has consumed it.”
She looks surprised.
“Ok, well, let’s get her off that,” she says and then lists on her bony fingers several nutrient-dense foods I would be thrilled for my daughter to eat but I’d be lucky to get my husband to try.
“Great!” I chirp. “How do I get her to eat all this?”
She looks at me blankly.
“We have a lot of trouble getting her to try new foods,” I explain. “Do you have any suggestions?”
“Just put it in front of her,” she replies, pulling out her phone because apparently we’re boring. “She’ll eat if she’s hungry enough.”
That’s when I knew it was all over. Because yes, most children will eat foods they don’t particularly like if the alternative is going hungry. But kids with sensory issues or oral aversions won’t, especially if they are too young or developmentally delayed to make the connection between hunger and food.
Her advice was the equivalent of Annie Sullivan telling the Kellers, “Just force Helen to develop a concept of language and a method of communicating.” Great in theory, but how do you get there?
In that instant it became apparent that, although this woman was well-versed in nutrition (she could correctly pronounce “quinoa”), she was pure JAGBA when it came to eating and the neurologically atypical.
I wasn’t alone in this assessment. A few months later, the neurologist added a feeding therapist to his staff so children could learn to eat these incredible diets being created for them.
And once again I was reminded that they can’t all be Sullivans.
In the grand scheme of things, it’s not that big a deal. Two years on and my daughter has almost caught up developmentally, even without the help of kale. Some people have asked why I even bothered with all the therapists and doctors if she would eventually get there on her own. The truth is, we had no idea if she would.
Also, as a parent you see your kid struggling with the basics and you want to help. You want your child to enjoy everything other children her age do: giggling with friends; the sweet, sunshiny taste of an orange; the pride of not crapping her pants.
Although there is far less call for Annie Sullivans around our house these days, I will probably always be on the look out for them. This is largely because I feel so out of my depth as a parent to the two unique, fabulous people that are my children.
So to any and all the Annies out there, thank you for what you do.
And call me if you have any suggestions.
This entry is dedicated to the miracle-working Ms. Lee. Thanks for being our first Annie Sullivan.